Audiology in Brief #2 - Dynamic Visual Acuity (DVA)


Why has your patient’s world gone blurry when they move their head?
How can you quantify this and monitor their rehabilitation?
Every day when we walk, run, and move our head, we want to maintain a clear picture of the world around us. What mechanism drives this?
Try this little experiment:
First – hold your thumb up 30cm in front of you and keep it still. Now move your head quickly back and forth, looking at your thumb. How clear is it?
Now – hold your thumb up again, and this time keep the head still and move the thumb back and forth very quickly. How clear is it?
In which situation is your thumb clearer? If your Vestibular Ocular Reflex (VOR) is working, it should be the first one.
The VOR’s primary function is to maintain visual acuity during movement.
In a normal functioning person, with the head is at rest, the neural firings from both labyrinths are equal. This lets the brain know that your head is not moving.
When the head moves to one side, neural firings increase to that side, and decrease on the opposite side. To keep the world from going blurry, the eyes move at the same speed as the head but in the opposite direction. This is controlled by the Vestibular Ocular reflex (VOR).
So, what happens in the case of a vestibular lesion? Straight after a lesion, the neural firings on the lesion side decrease, therefore the person perceives as though their head is moving to the opposite side even when their head is still. The patient feels quite dizzy and can have spontaneous nystagmus. However, this only lasts a few days with the body compensating quickly when the head is still. The patient will start to feel better as long as they don’t move their head. Over time with more compensation the patient will also start to improve with their head moving, this is Dynamic compensation.
So, how can you objectively assess the VOR system in response to head movement?
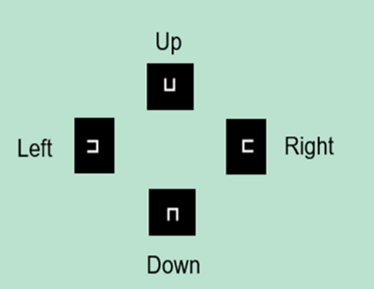
To assess VOR, you need to assess the patient with their head still and compare to while in motion. Using a device which tracks head movement with an IMU sensor, the patient is asked to look at optotypes and judge which direction it is pointing. The size of the optotype is decreased until the patient can no longer make a correct choice. This test is done with the head still and then while the head is in motion (horizontal and vertical planes). The computer measures the smallest optotype the patient can correctly identify. This can be done as a baseline test and again during the rehab process.
This information can be used to determine the level of vestibular compensation and to measure any improvements with rehabilitation.
If you already have the Visual Eyes system, DVA can be added as an additional test.
Keen on vestibular testing but don’t have the gear?
Why don’t you try a bed side measure first? You need very little equipment:
1. Snellen eye chart
2. Metronome app on your smart device
Have the patient sit in front of the eye chart with their head still and read the smallest line they can see (glasses can be worn, it is not an eye test). This is the baseline. Then moving their head at 2 cycles per second (2Hz), have them read the smallest line they can see (dynamic). In a normal patient, the difference between the baseline and dynamic visual acuity should be two lines or less. (In some patients with vestibular loss, it can be more than 6 lines).
Contact our Audiologists/Product consultants for more information.
Latest Articles
ABR Interacoustics Eclipse
ASSR and ABR Comparison on the Eclipse
